Sciatica is the term that refers to pain that radiates along the path of the sciatic nerve, which branches from your lower back through your hips and buttocks and down each leg. Sometimes the pain can run into the foot and into the toes.¹ Typically, sciatica affects only one side of your body. Sciatica most commonly occurs when a herniated disk, bone spur on the spine, or narrowing of the spine (spinal stenosis) compresses part of the nerve. This causes inflammation, pain and often some numbness in the affected leg.⁴ Although the pain associated with sciatica can be severe, most cases resolve with non-operative treatments within a few weeks.3 Treatment aims at reducing pain and restoring overall functional status.2
Signs and symptoms of sciatica
Common signs and symptoms of sciatica, include:
- Pain on one side of your buttocks or leg that worsens when you sit or stand for long periods, or when you sneeze, cough, or laugh;
- Burning or tingling feelings in your leg, foot, or toes;
- Weakness, numbness, or trouble moving your leg or foot; and
- Shooting pain that makes standing up hard.¹
Symptoms of sciatica include pain, stiffness, and/or soreness in the lumbosacral region of the back (underneath the 12th rib and above the gluteal folds). Pain may be considered acute (lasting less than 4 weeks), subacute (lasting 4 to 12 weeks), or chronic (lasting greater than 12 weeks).2
Causes
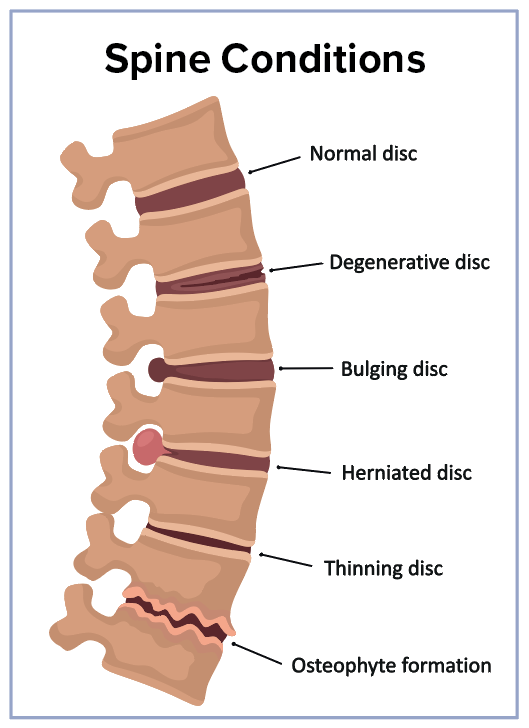
The exact cause of low back pain is often impossible to identify exactly, but arises from any combination of pathology involving intervertebral disks, vertebrae, facet joints, ligaments, and/or muscles.2 Sciatica is commonly caused by a herniated spinal disk (sometimes called a slipped disk) that presses on the sciatic nerve. A spinal disk becomes “herniated” when the gel-like center of the disk protrudes through the disk’s outer lining. It can also be caused by trauma from a car crash or fall, a tumor, injury to the sciatic nerve, or other conditions that put pressure on the nerve.¹
Complications
Chronic, ongoing, and lasting pain is a complication of untreated sciatica. If the “pinched nerve” is seriously injured, chronic muscle weakness, such as a “drop foot,” might occur. Some patients with sciatica may suddenly lose bladder or bowel control. If this happens, contact your healthcare provider immediately because it’s a sign of a rare but serious condition that needs emergency care.¹
Keys to prevention
- Exercise regularly. Exercises that focus on your core muscles in your lower back and abdomen can help prevent sciatica by supporting your back. Stretching exercises can help you keep flexibility and muscle tone.
- Watch your posture. Choose chairs with good lower back support, armrests, and a swivel base. Place a pillow or rolled towel in the small of your back to maintain its normal curve when sitting. If you work at a computer, adjust your chair so your feet are flat on the floor and your arms rest on the chair’s arms or the desk at a 90-degree angle.¹ Avoid sitting for long periods.
- Be careful when lifting. If you have to lift something heavy, keep your back straight, bend your knees, and use your legs to lift. Hold the load close to your body and avoid twisting and bending at the same time. Ask for help if something is too heavy to lift.
- Watch your weight. Maintaining a healthy weight within the recommended limits for your height can help you keep your back healthy. Excess weight can contribute to back problems.¹
- Avoid and stop cigarette smoking, which promotes disc degeneration. Some sources of sciatica are not preventable, such as degenerative disc disease, back strain due to pregnancy, and accidental falls.
Diagnosis
A complete medical history, including a review of your symptoms and a physical exam, can help the healthcare provider diagnose sciatica and determine its cause. Diagnosis of sciatica is made by eliminating specific lower back pain causes of neurologic compromise, neoplasia, inflammatory arthritis, fracture, or referred pain from other locations or organ systems.2 Other diagnostic tests might be performed to look for other causes of sciatic pain. Such testing might include:
- X-ray to look for fractures in the spine;
- Magnetic resonance imaging (MRI) or computed tomography (CT) scan to create images of the structures of the back;
- Nerve conduction velocity studies/electromyography (EMG) to examine how well electrical impulses travel through the sciatic nerve;
- Myelogram using dye injected between the vertebrae to determine if a vertebra or disc is causing the pain.⁴ However, most patients with sciatica can be treated without the need for further diagnostic testing.

Treatment
The goal of treatment is to decrease pain and increase mobility. Treatment most often includes limited rest on a firm mattress or on the floor, physical therapy, and the use of medicine to treat pain and inflammation. A customized physical therapy exercise program might be developed.
Avoid bending, lifting, or sitting in a low, soft chair. Staying in bed for long periods can make sciatica worse, therefore it is best to stay active.¹ Stretching exercises for your lower back, as directed by your healthcare provider, can help relieve pressure on your sciatic nerve. Walking, yoga, and pilates are good exercises for sciatica.¹
©2022HealthSpot References: (1) Nursing 2011. Patient education series: sciatica. Lippincott Williams & Wilkins. https://www.nursingcenter.com (Accessed on January 22, 2019.) (2) Epocrates Essentials. Musculoskeletal lower back pain: highlights and basics. Athenahealth, Inc. https://online.epocrates.com (Accessed on November 19, 2018.) (3)Jobson MD. Second-generation antipsychotic medications: pharmacology, administration, and side effects. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc. http://www.uptodate.com (Accessed on November 19, 2018.) (4) Mayo Clinic, 2018. Sciatica. https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435 (Accessed on November 19, 2018.)

